Research should lead to real-world impacts, not just publications. Therefore, researchers should consider scalability and sustainability from the outset, as these are key to lasting change. These are among the top issues that resonated across conference presentations, plenaries, and special sessions at the 2025 Health Systems Innovation Conference (HSIC) held at the University of Ghana, Legon. Conference attendees highlighted the need for continuous engagement of all relevant stakeholders at all levels of the health system in projects from the beginning to the end if knowledge is to be effectively translated into action.
The Health Systems Innovation Conference was jointly organised by the Regional Institute for Population Studies (RIPS) and the Ghana Health Service (GHS) as part of activities under the Sustaining the African Health Initiative Community of Practice (AHI CoP) project funded by the Doris Duke Foundation (DDF). The project’s goal is to improve population health through system-wide interventions and generate knowledge that can be scaled across Africa. The two-day conference contributes to the development of resilient and equitable health systems capable of effectively responding to current and future health challenges. The conference thus focused on showcasing cutting-edge research and innovative solutions that can be scaled to sustainability to address health systems challenges; building and strengthening multisectoral partnerships; influencing health policy through evidence-based recommendations; fostering dialogue between researchers and policymakers; and promoting inclusive health systems innovations that address the needs of vulnerable populations.
Under the theme “Advancing Evidence-Based Innovations for Strengthening Health Systems in Africa,” the conference assembled 176 researchers, policymakers, and health practitioners from 15 countries across Africa and collaborative institutions outside the continent. Through keynote speeches, panel discussions, oral and poster presentations of research findings, and networking sessions, both in-person and online, participants called for increased domestic health financing and partnerships with state and non-state actors to strengthen inclusive, community-based healthcare systems. They advocated for local ownership and sustained community dialogue and leadership engagement to increase women's participation in healthcare governance.
Whereas the Deputy Director-General of Ghana Health Service, Dr. Caroline Reindorf Amissah, represented the Director-General of the Ghana Health Service as Chairperson of the Opening Ceremony of the conference, Dr. Samuel K. Boakye-Boateng, Director of the Policy, Planning, Monitoring, and Evaluation Directorate at GHS, made the closing remarks on behalf of the Director-General. He stated that researchers, policymakers, and health practitioners working together are more than a community of practice; they are a force to reckon with in efforts to scale innovations for sustainable impact. Dr. Boakye-Boateng highlighted participants’ “active participation, insightful contributions, and commitment to evidence-based research” as critical for strengthening health systems in Africa.

The keynote speaker for the opening ceremony, Dr. Koku Awoonor Williams emphasized Ghana’s pioneering efforts in community health services, particularly through the GEHIP and CHPS+ programs, which have significantly improved access to primary healthcare across rural communities. With the integration of mobile health technologies, digitalized health insurance services, and modern emergency response platforms, Ghana is strengthening its healthcare framework to ensure equitable, sustainable, and impactful health solutions.
Presentations on the role of Digital Health and Telemedicine in bridging gaping healthcare gaps emerged among the most forward-looking innovations for improving community health, especially in hard-to-reach localities. Bridget Setorrnyo Letsa’s presentation on the role of telemedicine in bridging the healthcare gap in the Hohoe Municipality of Ghana using the Hub and Spoke Model highlighted the significant improvement in healthcare accessibility. Telemedicine services provided by the Teleconsultation Centre (TCC), including consultation, counselling, follow-ups, reminders, and functional linkage, were particularly useful in rural areas. She explained that the Teleconsultation Centre links community-level cases to higher-level facilities through phone consultations involving various healthcare professionals, such as doctors, nurses, and midwives. She noted that two out of every five TCC-managed cases related to maternal health, one out of four on non-communicable diseases, and nine out of ten complex cases were referred to higher level facilities. “This TCC model has been particularly effective in reaching remote communities, with a significant number of cases, notably maternal health, being managed through audio-based consultations,” she said and called for the development of video calling capabilities to augment the audio communication of the TCC to improve its work.
Results of Nana Mireku-Gyimah’s innovative Home Visit App, developed using Kobo Collect and integrated with Microsoft Power BI, piloted in Mpohor-Fiase District in Ghana, showed improved monitoring of home visits, increased follow-up on vaccine defaulters, leading to better maternal health outcomes. Addressing concerns about the frequency, cost, and scalability of the Home Visit App, Nana Mireku-Gyimah stressed the App’s flexibility, data privacy measures, and the need for adequate infrastructure and funding to bring the innovation to scale.
Agoligan Tometin Nihad’s presentation on gender intentionality in Benin’s Assurance Maladie pour le Renforcement du Capital Humain (AM-ARCH) health financing reform concluded that although the scheme offered inclusive services, it fell short of gender-responsive budgeting and failed to involve gender experts in planning, monitoring and evaluation. However, the absence of sex-disaggregated data and weak institutional frameworks limited the ability to track and address gender disparities meaningfully in healthcare delivery.
Eunice Tangwam’s study on improving first-trimester pregnancy registration at Kologo Health Centre in the Kasena-Nankana Municipal of Ghana demonstrated how small, local initiatives can significantly improve maternal health. She said targeted strategies such as registering pregnant women during scan wait times, engaging Traditional Birth Attendants and community leaders to encourage early ANC visits, conducting follow-up visits, and introducing urine pregnancy tests (UPT) at the outpatient department (OPD) helped reduce delays and increase early ANC registration from 33% to 60% within three months. Despite insufficient UPT kits, difficulty mobilizing TBAs, and the additional workload required to sustain interventions. She was emphatic that “the introduction of UPT at OPD enabled early pregnancy detection and timely referral for care” and should be scaled.
A special session was dedicated to mentees on the AHI CoP and early-career researchers. When asked what challenges they face in their work, early-career researchers bemoaned bureaucratic barriers to data access, lack of institutional support, and skill gaps, all of which impede their professional development. Farrukh Ishaque Saah of the University of Cape Coast disclosed that institutional or secondary data, which could have complemented his study of perinatal mental health screening, could not be obtained because of bureaucratic processes. Mercy Adjei Adumatta of the University of Health and Allied Sciences (UHAS), lamented the general lack of support from the health facilities, which not only made it more challenging for early career researchers to reach potential respondents, but also unnecessarily prolonged data collection. Attipoe Woelinam Aku also from UHAS, advocated capacity-building workshops for early-career researchers to improve and sharpen their skill set. The chairperson for the session, Pearl Kyei, commended the diligence of early-career researchers and singled out for special mention the study on mental health for addressing a sensitive yet crucial issue. She called for institutional backing for early-career researchers and pledged ongoing professional development for early-career researchers through the RIPS webinar series.
Two presentations on health systems strengthening, lauded as innovative, explored how strategic reforms, whether at the macro-policy level or within individual health institutions, can contribute to improved health outcomes and system sustainability. Whereas Idrissa Ouedraogo’s presentation focused on the broader institutional and policy context, analysing how economic freedom shapes health capital development, Leonard Naphazi Kambewa’s provided a more practical, facility-level perspective of an innovative financing model implemented at Phalombe District Hospital in Malawi to address severe budgetary gaps. To further enhance the policy relevance of the two studies, discussants recommended the need for Idrissa Ouedraogo’s study to link economic freedom to macro-level health outcomes such as life expectancy. They also urged Leonard Naphazi Kambewa to elucidate how micro-level factors interact with economic freedom to influence health. The two presentations highlighted the importance of structural reforms and context-specific innovations in ensuring equitable, resilient, and financially sustainable healthcare in Africa.
Other potentially scalable research works included the Network of Practice model delivered through Model Health Centers and their supporting facilities, and the need for policy revision to broaden Physician Assistants’ prescribing authority to optimize service delivery; the Community Scorecard Initiative, a social accountability tool implemented designed to amplify community voices, improve healthcare service delivery, and strengthen health governance; and Abdul-Jaleel Mumuni’s Data Envelopment Analysis (DEA) for improving the operational efficiency of CHPS compounds. Michael Yaw Amoakoh’s Lightwave Health Information Management System on healthcare services contributed to improved efficiency and patient record management. The researcher called for urgent action to strengthen IT infrastructure and technical capacity to enhance the effectiveness of electronic health records.
Whereas the conference afforded most participants the chance to showcase their groundbreaking research, it enabled others to improve the science in their area of research. The presentation on supply chain management and patient satisfaction showed potential to guide policy and practice, for which discussants suggested further analysis to sharpen the recommendations.
It was noted that, where investments are made or solutions proposed without the full picture, particularly when communities, researchers, or other important players were not consulted, leads to wasted resources and missed opportunities. Participants noted that resentment and supply chain disruptions can occur when those working behind the scenes on policy are not acknowledged as the main drivers of that policy. “There is the need for inclusive dialogue, shared ownership, and transparency early on to prevent future disconnects and ensure sustainable outcomes,” a participant suggested.
Across all presentations, common challenges in building resilient health systems across Africa included logistical constraints, insufficient training, gender gaps, and resource disparities. The recommendations emphasised regular refresher training for health workers, gender mainstreaming in policy implementation, locational targeting in resource distribution, and the integration of private and community-based schemes into national health systems. Collectively, the insights offered practical strategies for enhancing primary healthcare implementation and achieving Universal Health Coverage in Africa, reinforcing the need for inclusive, data-driven, and gender-responsive health systems that can be scaled and sustained.
Using Ghana’s flagship pro-poor health policy, the Community-Based Health Planning and Services as a case study, Prof. Ayaga Bawah, Director of RIPS at the University of Ghana, and the Principal Investigator of the AHI CoP project, highlighted a multi-faceted approach to health system strengthening, underscoring the need for local ownership, context-specific solutions, and continuous learning to achieve sustainable health outcomes. He urged conference attendees to focus on community-driven resource mobilisation as they helped improve the science and broaden the evidence base for health policy decision-making.
The 2025 Health Systems Innovation Conference came to a close with the lingering feeling that the nature and extent to which climate change influences health systems are yet to be fully understood and appreciated. There were no abstracts on Climate Change and Health Systems as one of the eight themes of the conference.
A minute’s silence was observed at the closing ceremony in memory of Lola Adedokun, former Director of the AHI at the Doris Duke Foundation, who strongly advocated for embedded implementation research to strengthen health systems and promote the dissemination of lessons learned from the AHI during her lifetime. She passed away in 2024.
The closing ceremony also featured the presentation of the awards to the best poster presenters for the conference and a special acknowledgement of the early career scholars whose papers were accepted for the conference.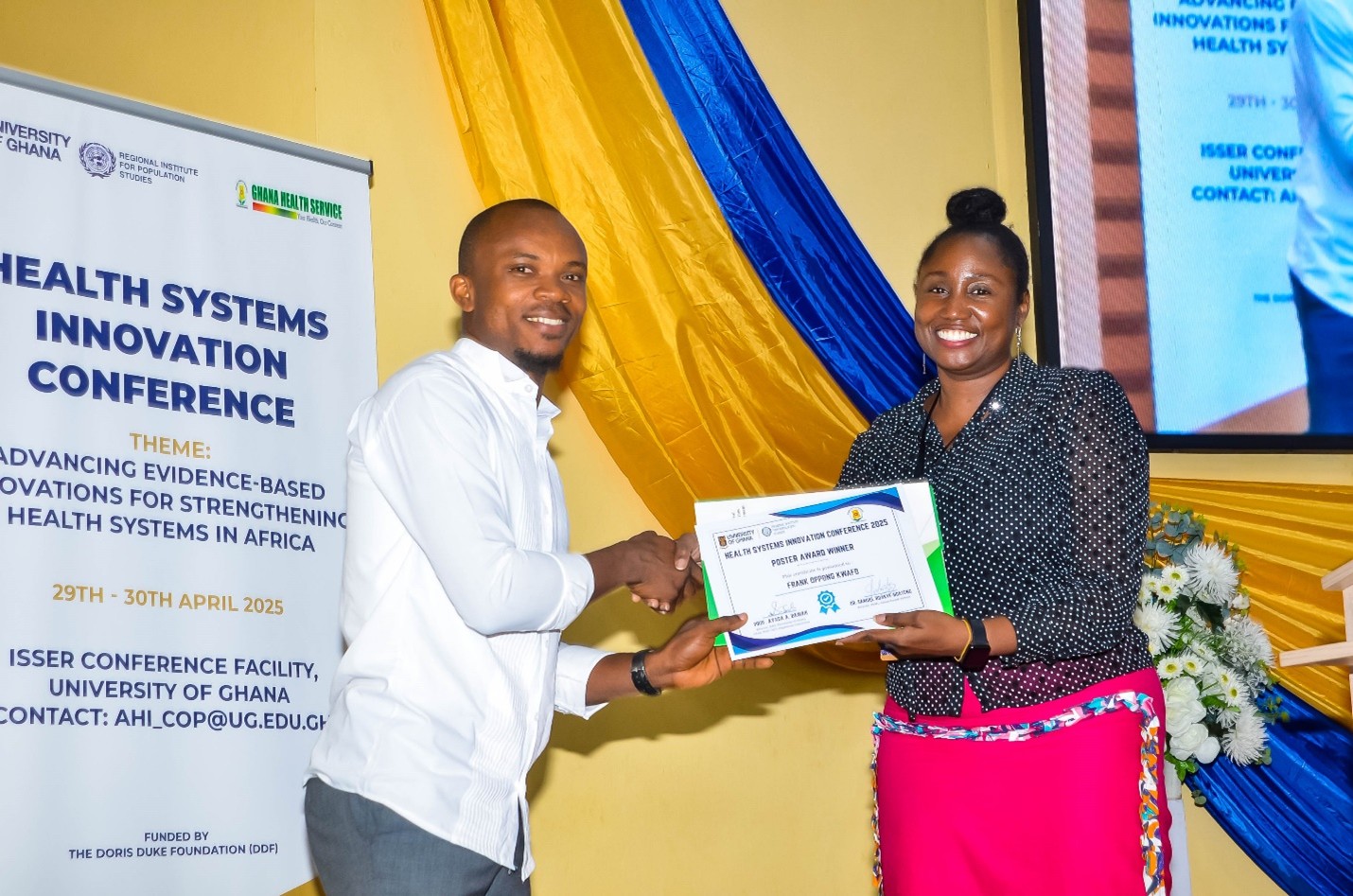
For more information on the presentations at the conference, download the book of abstracts
Read more articles
- Log in to post comments


